PART ONE of this article on sleep dealt extensively with the reasons for prioritising high quality and sufficient sleep. In summary, there are substantial gains in performance and health vitality as well as warding off the most serious health concerns connected to ageing such as cardiovascular disease, cancer, stroke and dementia. This article deals with how to sleep better when you have insomnia.
Getting just four to six hours a night on an on-going basis won’t kill you today but over time this sleep deficit can create a cascading problem where the body becomes unable to maintain a healthy temperature or weight, and where infections run rampant due to a suppressed immune system. All known mental health conditions correlate to poor sleep.
This article also draws heavily on the latest sleep research outlined, especially “Why We Sleep” by sleep researcher Matthew Walker, as well as my own clinical work.
SLEEPING PILLS ARE A FALSE GOD
Whilst most of us don’t get enough sleep, we do value it enough to ensure that we take steps to get at least some sleep. The most common way for us to address poor sleep is, perhaps, the least effective, through sleeping pills.
Firstly, in important ways, sleeping pills don’t help you sleep, they sedate you. Sedation and sleep are very different. Sleep is an essential, active, process required by every animal ever studied. In the higher mammals and birds, for instance, the sleep process includes cycling through the day’s experiences to decide what to delete and what to keep. For an adult human, this elaborate dance through REM and non-REM sleep takes a full sleep cycle of around eight hours to complete. During this period, your resources are also used to remove detritus from the brain, to replenish and heal the body.
Throughout the sleep cycle, the brain may actually be more active than when awake. Between a quarter and a half of your natural brain-wave sleep cycle is lost when you take a sleeping pill. Sedating your neurology is sabotaging its restorative mission.
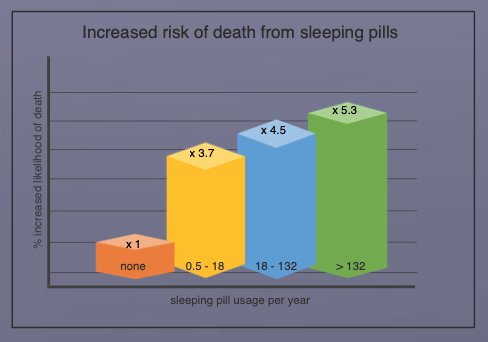
Secondly, sleeping pills are really dangerous, even when taken as prescribed (see chart). According to Walker, common sleeping pills such as Zolpidem or Ambien: “…. lead to grogginess, poor function, forgetfulness, slow reaction times – with the benefit being more subjective than real. People taking sleeping pills [in this extensive study] were 4.6 times more likely to die than those not taking the pills; infection was a common problem because the body’s immune system is therefore compromised.”
Of course, any lack of quality sleep has two potential causes, “won’t” and “can’t”. Many of us won’t prioritise sleep, deciding instead to stay up a little later and hoping that when the alarm clock wakes us up we won’t feel too bad the next day. But there’s also a large slice of the population that, try as they might, can’t sleep – the insomniacs.
WHAT IS INSOMNIA?
Everyone is born with the ability to have deep refreshing sleep but clearly some people are better at it than others. Babies raised in noisy environments learn to sleep through most things. When parents protect their babies from all noise and chaos at night, they tend to suffer more as adults and wake at the slightest environmental noise.
For those who do struggle to sleep as adults, there are two types of insomnia: onset and maintenance insomnia. Those with onset insomnia just can’t get to sleep; those with maintenance insomnia just can’t stay asleep. Sufferers tend to toss and turn all night, awake with an active mind, tired but unable to drift off.
Identifying the true cause of insomnia can be difficult. Unlike most conditions, the possible causes of insomnia are truly manifold. Initially, let’s talk about each of the more minor factors known to cause insomnia before we talk about the elephant in the room – anxiety.
There are essentially four pillars to a healthy sleep, to the extent that any of these pillars cannot support sleep, the others might need to work harder, or healthy sleep might become impossible. These pillars are medical, environmental, physiologically and psychological.
MEDICAL REASONS FOR INSOMNIA
If you suffer from insomnia on a regular basis and you’ve addressed the other pillars in this article it’s essential to have your physical health checked. There are many serious health conditions, often arising later in life that can cause insomnia. Conditions such as diabetes, sleep apnoea, asthma, etc. can go undetected for years and can have a substantial effect on your ability to sleep. Similarly, conditions such as arthritis and chronic pain will interfere with sleep and every effort should be used to minimise their impact on your life so that sleep improves.
Ageing brings its own problems. Our susceptibility to stimulants changes so, for example, the dinner expresso that used to cause no problems in our 30’s can become an issue later on. The human brain includes substantial redundancy built-into its network and can continue to function despite the cumulative damage to the network caused by ageing. Rather than suddenly stopping, it degrades slowly. Like the ‘boiling the frog’, we often don’t notice the small increments that lead to big differences over time. We’re not the same person we were when we were young. In particular, areas of the brain associated with monitoring the daily circadian cycle can become less sensitive to the melatonin release that usually helps us wind-down and sleep at night. For this reason, some seniors may benefit from taking melatonin and should discuss this with their doctors; it’s not usually helpful for the rest of us. Seniors might also find it more helpful to get sunlight exposure at times of the day that can train our body clocks because they are less able to take the cues from the environment later in life. In other words, getting all your sun exposure late in the day is unhelpful if you’re struggling to sleep.
ENVIRONMENTAL REASONS FOR INSOMNIA
This pillar is somewhat peculiar to the insomniac. People have different sensitivities and this can be noise, light, temperature, comfort, etc. These problems tend to be much worst when a person is more restless due to anxiety since this raises a person’s level of vigilance. Again these sensitivities can change over a person’s lifetime. Use the Sleep Hygiene Checklist here to ensure you’re not falling foul of the usual suspects.
It’s worth noting here that a bed-time routine is a worthwhile part of good sleep hygiene. Going to bed and getting up the same time every day, even weekends has been shown to improve quality of sleep. Early exposure to the sun in the morning is great, followed by reducing light exposure in the evening. Soft yellow lighting should replace white lighting at night. Listening to music can also be good to help you wind down if you’re not relaxed. Exercise should be part of every day to encourage physical tiredness but not just before bedtime. If you’re not sleepy after 15 minutes, get out of bed until you are and then go back to bed when you’re more tired.
Don’t watch the news in the evening if there’s any chance it will annoy or worry you. Avoid shift work like the plague; it’s terrible for you in every conceivable way. If you’re committed to shiftwork, don’t search the internet for research in this area, you’ll never sleep again. Honestly, don’t do shiftwork!
Sleep Hygiene Checklist
- TV’s, phones, tablets in the hour before bed. The light shining in our eyes makes our brains think it’s daytime. Put your phone in another room.
- Curtains/blinds that let light in. Your bedroom should be too dark to see anything once the lights are off. Blindfolds or black-out curtains can help.
- Neon-lights on alarm clocks, sockets, appliances, etc. Unplug, cover or turn them away from you.
- Lazy laundering. Cool, comfortable bedding, cleaned regularly.
- Cool room! Your body needs to cool 2o to sleep. Aim for a warm bed but a cool room, around 65oF (18.3oC). Your limbs should easily be able to escape the bedding to help you cool without waking you.
- No air. Fresh air is essential. If you can’t open the bedroom window, can you ventilate the room another way?
- Noisy neighbours. Try to reduce noise. If you can’t, a white-noise generator might help conceal the noises. (There’s an App for that!)
- Stimulants. No caffeine in the ten hours before bed.
- No red wine due to tannins. Nicotine is a stimulant!
PHYSIOLOGICAL REASONS FOR INSOMNIA
The physiological state that we are in when we go to bed will obviously have an effect. Running around, arguing, playing loud anthemic music, exercising, eating a meal, etc. just before bed is a dumb idea if you want to sleep. In the same way you want to get a child to sleep, you create an activity slope, a routine, downwards, toward a comfortable stillness. Being tired is helpful, so there should be physical activity in each day even if it’s just an energetic 20 minute walk earlier in the day. To get the most benefit from daily fatigue, don’t take naps after 3pm.
That tiredness from mental and physical exertion is useful, yet we often try to fight tiredness during the day through stimulants. Having stimulants in your system is a terrible idea if you’re trying to sleep. Stimulants keep our external awareness turned on – the last thing you need if we’re trying to sleep.
“But I haven’t taken anything for hours!”, I hear you say. The half-life of caffeine can be around five to seven hours, so it’s still having around a quarter of its initial effect up to fourteen hours from when you took your last drink. Even a small amount of most stimulants is more than enough to keep an insomniac awake. So, if you’re regularly sleeping poorly, lunchtime is probably the latest you can safely take any common stimulant, like coffee, tea, certain foods (including chocolate). It’s worth mentioning too that even decaffeinated tea doesn’t mean caffeine-free. Some insomniacs will need to remove all stimulants to get a healthy sleep.
There are other common, yet more hidden, stimulants, especially some types of alcohol. Smoking is not good. Nicotine is a stimulant; it triggers the release of adrenaline in a desperate attempt to remove the 500 poisonous substances you just put in your body. “It can’t be the cigarettes…”, I hear you say, “… I smoked for years and I slept fine!” But denial won’t help you sleep; remember, you’re not who you were when you were 18. Ageing reduces your body’s ability to remove these chemicals, thereby increasing the half-life.
For those that think that alcohol helps them sleep, it bears emphasising that whilst alcohol, on the whole, is a sedative, the sedation of your neurology is not proper sleep (see Sleeping Pills above). As the sedation wears off, the drinker often wakes, leaving the person still unable to sleep due to the underlying cause but now also fighting all the problems alcohol withdrawal brings as well as any stimulating effects. Red wine, in particular, often has this initially sedating effect, followed by a longer- lasting stimulant effect which confuses and encourages self-defeating behaviour. Drinking more, makes the problem worse, whilst giving the impression it’s helping.
If you’re on any daily medication, check the side-effects to see if this could be the cause of your insomnia. Many over-the-counter and prescription medications can affect your physiological state before bedtime. Pain and cold/flu medications, especially anything with ‘extra’ in the title, usually includes a stimulant. Medications that act on your cardio-vascular system or your hormone levels can often affect sleep. Serotonin is one of the key neurotransmitters associated with sleep regulation and this is a key target for many anti- depressants, with unpredictable results. Many people on these drugs don’t get the symptom relief they’re looking for, so remain anxious and depressed, whilst also fighting the side-effects of the medication.
There are often better ways of dealing with these conditions, see below.
PSYCHOLOGICAL REASONS FOR INSOMNIA
Anxiety is the mother of all sleepless nights. Most of us are aware of ‘fight, flight and freeze’ experience created by our amygdala in response to a perceived threat; the sudden increase in heart-rate, the sweaty palms, the sick feeling in the stomach, chest, neck or head. The release of adrenaline is central to this process and, in addition to the above, it also increases alertness and vigilance as well as reducing the effect of fatigue.
Of course, there typically aren’t that many immediate threats to respond to when we’re tucked-up in bed. But our body responds to our thought stream, so in addition to any threat registered by our senses, our amygdala can also be triggered by a memory (trauma) or from our imagination (anxiety). Whilst these stressful thoughts continue, we are easily triggered into external alertness rather than to be sensorially absorbed by the comfort of your warm bed.
Sufferers of anxiety and depression have traumatic experiences from the past and the imaginary future running in the background or foreground of their consciousness. The worrier may tend to over-prepare for future events, conversations, eventualities, emergencies. They often lack the confidence in their inherent abilities to deal with whatever arises, as it arises.
Significant traumatic events often predict the onset of insomnia. This can include an accident, health scare (you or an acquaintance), assault, loss of job or status, break- up and, of course, a death. Post-Traumatic Stress Disorder (PTSD) includes constant re-living of traumatic events, an inability to sleep, hyper emotionality and vigilance. Most of us have gone through certain events where this seems familiar, often to a lesser degree than the soldier on the front line who is often associated with the condition. Really the soldier’s suffering is just a more extreme version of common anxiety, activated by a more extreme experience.
Trauma (the past) and anxiety (the future) go hand in hand, one creates the other, but usually, people have a preference. Once established, either problem feeds into a vicious cycle of insomnia. Our lack of sleep reduces our ability to clear trauma from the system (see Part I, Sleep – The Easy Road to Improved Mental and Physical Health). The worse our sleep, the lower our resilience and the worse our ability to recover. The opposite is true too, improved sleep helps to resolve emotional issues and promotes strong mental and physical health.
There is some suggestion that anxiety conditions tend to happen more often to those that have such events in early childhood, especially the loss or estrangement of a parent, constant fighting, etc. It’s as if the person’s neurology says, “Well if this is what life’s like, I’d better expect the worse, prepare for any eventuality and really keep my eyes peeled.” Sleep is naturally more difficult under these circumstances because the mind stays in threat mode. The mind cannot disengage from the ruminative brain activity. This again is an area where good therapy can help. Once the trauma is dealt with, the associated problems tend to go away and a natural sleep cycle returns.
GET SOME THERAPY
Insomnia can be beaten. If you need help, book a session with a cognitive hypnotherapist. These therapists are experts in sleep, relaxation and anxiety conditions. Understanding the subjective mental experience of the client is an area which most other therapies don’t consider in the same way. Once any underlying therapy issues have been sufficiently addressed, the treatment may include psycho-education, an assessment of sleep hygiene as well as a hypnotic recording, designed especially for you, to help you get to sleep.
Contact me today, if you’d like me to help you address your sleep problems.
Other Helpful Resources
- Why We Sleep’ by sleep researcher Matthew Walker (2018). An excellent summary of sleep and insomnia research, which has heavily influenced this article.
- ‘Sleep–The Easy Road to Improved Mental and Physical Health’ – Part I of this article, by cognitive hypnotherapist Simon Bates, drawing on current research and years of experience helping people to sleep better.
- ‘I Can Help You Sleep’ by Paul McKenna. An accessible self-help book on insomnia with excellent sleep hypnosis track.
- www.qchpa.com find a cognitive hypnotherapist to help work through issues of sleeplessness.


Recent Comments